The Endemic Epidemic
Madagascar’s Struggle with a Strain of Europe’s Past
Though the epidemic is common in Madagascar, an unprecedented outbreak of the plague in July has swept from the remote country into densely populated urban centers. Cities Toamasina and Antananarivo have attracted foremost attention, being the nation’s leading economic centers in the trade and fishing industries, and the latter, Madagascar’s capitol.
However, the so-called “Black Death” of olden times is not the threat of modern day. Instead, the impetus for the current crisis has been identified as an offshoot strain—plague pneumonia.
Pneumonic plague is more dangerous, characterized by its ability for person-to-person transmission, such as with coughing or sneezing. This disease is unique in that it stems from an intensified case of bubonic plague, when an infection enters a patient’s lungs through the respiratory system. However, plague pneumonia is distinguishable by general symptoms. These include high fever, headache, chills, and fatigue.
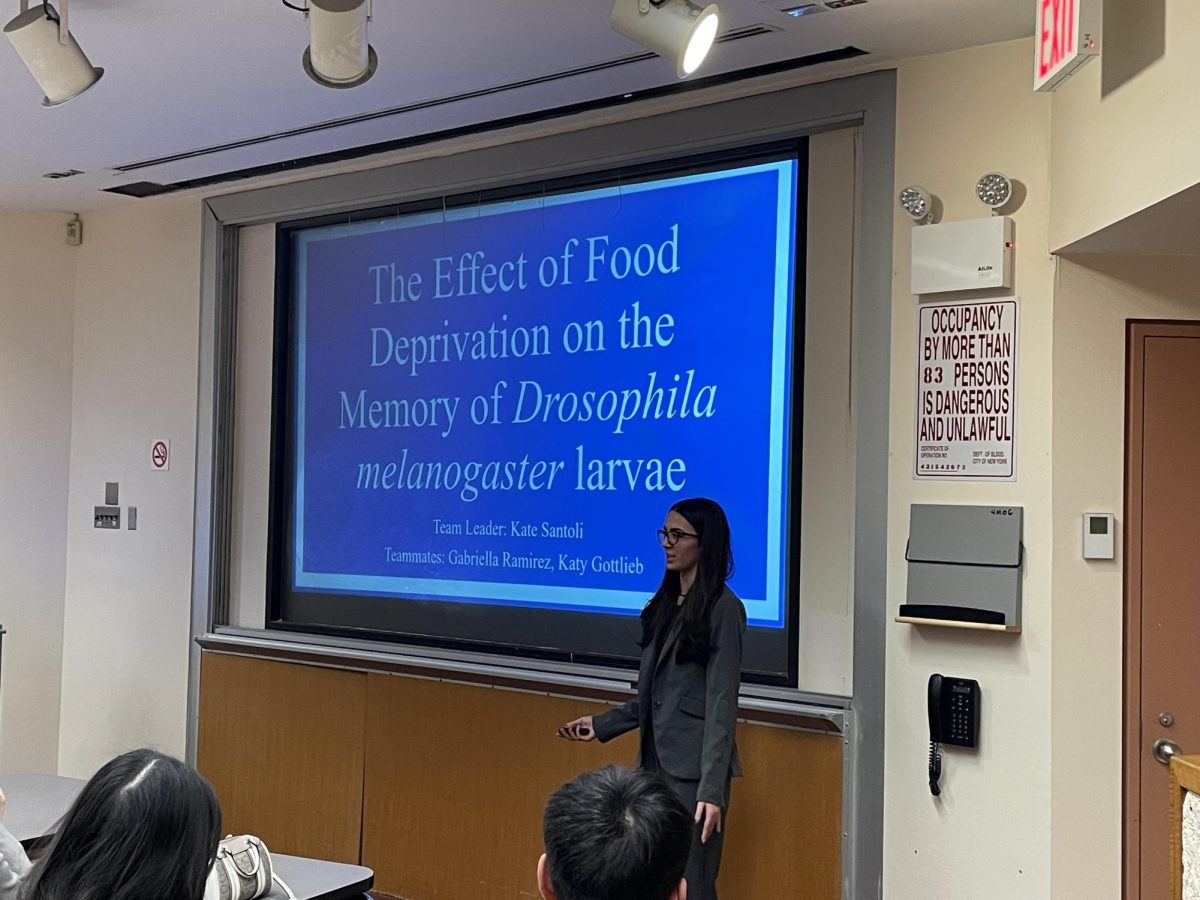
Social Studies Teacher Olga Zisel, whose familiarity with the disease lies in historical fact and curriculum, also shed light on the plague’s past. “In the High Middle Ages of Europe, a rising merchant class led to a rise of trade. European trading ships brought back the rats who carried the bacteria, Yersinia pestis. In Europe, almost half the population died in a few short years, mainly due to the fact that they had no interest in hygiene, since it wasn’t a priority during a dark time in history,” Zisel stated. “This is happening currently on an island, but it is also concerning if it were to spread on the mainland of Africa. If people are in close contact with one another, and the disease is also airborne, it’s difficult to avoid in a country where you have poverty stricken areas with rats and poor sanitation. It could be difficult to control, and access to antibiotics may lessen, as more people become infected.”
Already, countries linked through trade to Madagascan ports have been cautioned to increase public surveillance, if only to raise awareness of the plague’s dangers. Nevertheless, the World Health Organization (WHO) has described the risk of further spread as “very high”—giving the nations of Seychelles, Mauritius, South Africa, Tanzania, Le Reunion, Mozambique, Kenya, Ethiopia, and Comoros reason to worry.
Of Madagascar’s 114 districts, the United Nations Office for the Coordination of Humanitarian Affairs has reported 40 with pneumonic plague, with less than 30% of cases having contact with traceable sources. Thus, those who have been to the region recently, particularly tourists and foreign aid workers, are highly encouraged to seek medical care as soon as possible.
In a statement to CNN, Tarik Jasarevic, a spokesman for the World Health Organization (WHO), noted that when “compared with past outbreaks, this year there is higher portion of pneumonic plague cases.” Since plague is found regularly in Madagascar, its “spread to non-endemic areas which were not used to handling plague cases, including densely populated cities,” may have caused a more severe outbreak.
To stem the loss of life, WHO has stockpiled enough medication to treat upwards of 5,000 people, and protection for the nearly 100,000 people who may have received the disease through an exponential spread. The Red Cross has made similar moves, announcing future deployment of treatment centers, with the organization’s Secretary General Elhadj As Sy launching an emergency appeal for about $5.5 million.
According to one study conducted from the beginning of August into late October, 1,836 possible cases of the strain currently exist. Of that number, 61% are likely plague pneumonia; the current death toll now 133.
Although, the WHO has described the disease’s destructive trend to, in fact, be “relatively stable,” one point in reference to curbed growth of the disease from 477 new cases on October 9 to 161 on October 23.
The Madagascan government has likewise characterized unsettling health figures as misleading—stating that approximately half of all current deaths occur within the victims’ local communities. Thus, it has been made imperative that government officials publicize treatment for the disease at existing health centers.
Still, it will be hard to shake an undercurrent of cynicism felt towards the country’s government, caused by continual interference in the affairs of preexisting tribal customs. Not surprising, given the promotion of ancestor worship evident in the nation’s motto alone (“Love, Land of Our Ancestors, Progress”).
In relation to investigations conducted under a variety of health organizations, specific attention has been given to Madagascar’s central highlands: the region identified as the source of the outbreak’s patient zero, a visiting 31-year-old who developed malaria-like symptoms four days prior to his death.
Responding to allegations from the medical community, local officials have pointed toward the unorthodox: the funerary tradition of famadihana, or “body wrapping.” Believed to have existed as part of tribal culture well before the 17th century, annual famadihana ceremonies call for the exhumation of the deceased, following by dancing with the freshly wrapped bodies of the dead before returning them to their graves.
To prevent the chance of further flare-ups, new health protocols dictate that plague victims be buried in anonymously chosen mausoleums, rather than risk the accessibility of private tombs. Many, however, are reluctant to let go what is a sacred ritual.
“I don’t want to imagine the dead like forgotten objects. They gave us life,” Helen Raveloharisoa, a regular of famadihana ceremonies, said in an interview with Newsweek. “I will always practice the turning of the bones of my ancestors—plague or no plague. The plague is a lie.”
I am a sophomore contributor to Horizon, a New York resident since 2002, and child of the New Millenium.